Articles
Breast Reconstruction After Mastectomy
Surgery for breast cancer
Breast cancer is the number one cancer amongst women. Thankfully, treatment options for breast cancer have advanced tremendously, whereby most women with breast cancer can expect to make a full recovery. These options include surgery and adjuvant therapies such as radiotherapy and chemotherapy, with surgery as the mainstay of treatment for breast cancer. Surgery for breast cancer includes partial resection, full resection (also known as mastectomy), and surgical management of the regional lymph nodes.

Partial resection generally means wide excision of the tumour with margins. Depending on the size and location of the tumour, this may extend to a quadrantectomy, where up to a quarter of the breast is excised. Very often, partial resection options require post-surgery chemotherapy or radiotherapy to help in treating the rest of the cancer field.
In the past, full resection/mastectomy options were limited to simple or radical mastectomies, where a large portion of the breast skin was removed, occasionally along with the underlying chest muscles. With improved knowledge of breast cancer and adjuvant therapies, mastectomy has evolved to muscle-sparing, skin-sparing, and even nipple-sparing mastectomies. With the latter, the mastectomy scar can be hidden in the inframammary fold of the breast or be performed via minimally-invasive laparoscopic or robotic approaches.
Surgery for breast cancer also includes a treatment of the regional lymph nodes, most commonly in the axillary (armpit) basin. This can be just a simple sentinel lymph node biopsy, or complete axillary clearance of lymph nodes if a more extensive spread is found or suspected.
In the modern management of breast cancer, surgery cannot be discussed in completion without offering breast reconstructive options. This truly provides holistic and full recovery to normal for the patient.
Why is breast reconstruction surgery important?
The breast is considered part of a woman’s full normal anatomical structure. Breast reconstruction after mastectomy/partial breast resection helps to restore this whole. Currently, most breast reconstruction options aim to restore form and symmetry to women, along with some sensory function. This allows women to return to a normal life of activities, including exercise, going to the beach, and wearing well-fitted undergarments. Multiple studies have shown that breast reconstruction after mastectomy improves the quality of life in women versus those who do not receive reconstruction. In addition to the quality of life, psychological well-being returns to normal as well.
Another important contribution of breast reconstruction surgery is the management of lymphedema, which is arm swelling after breast cancer treatment. Whilst this can dictate a whole other article, it is important to note that around 30% of women who receive breast cancer treatment develop lymphedema in the arm of the involved side. Lymphedema treatment and surgery can be instituted at an early or later stage to help with preventing and reducing the debilitating effects of lymphedema.
What options are there for reconstructive surgery after breast cancer?
Reconstructive surgery after breast cancer can be performed immediately after the resection or mastectomy during the same surgery or later in a delayed reconstruction. The latter is usually done once all adjuvant therapies have been completed. In some cases, a hybrid approach can be taken, whereby a temporary tissue expander is placed at the time of resection and volume is gradually added after the adjuvant therapies to enable a more native skin envelope to be available at the time of final reconstruction.
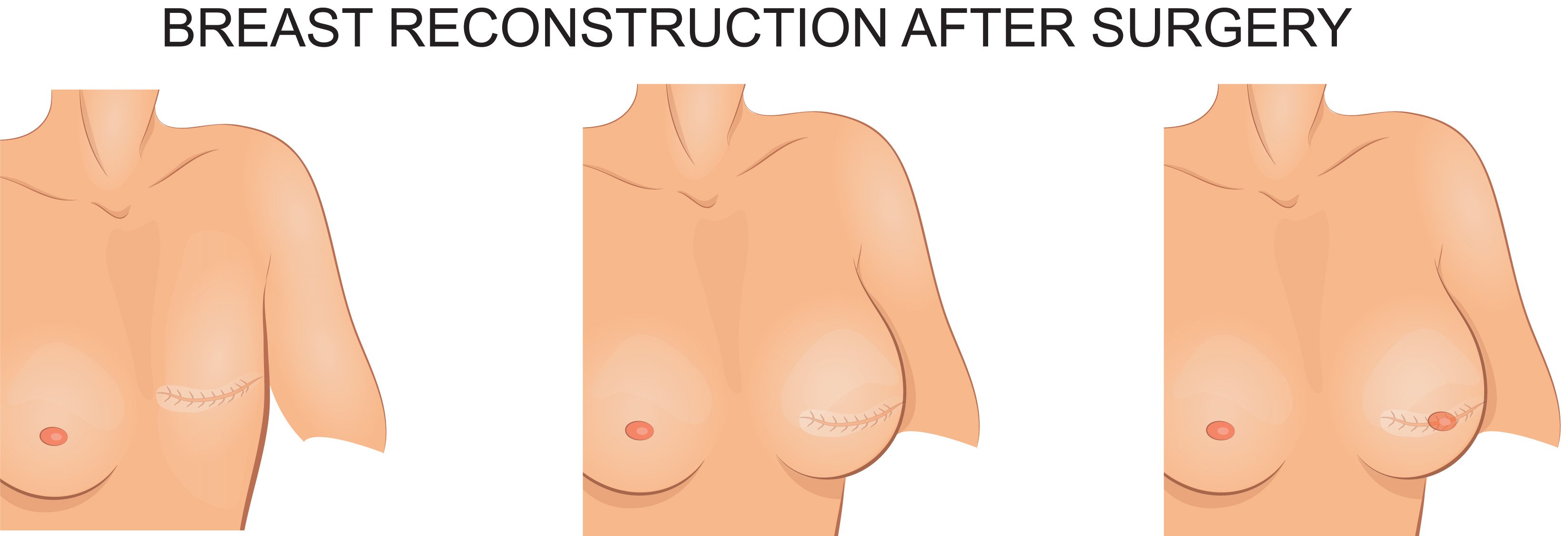
The types of reconstruction are generally divided into implant-based and own tissue (autologous) reconstruction. Occasionally, both techniques may be combined to help improve reconstructive outcomes.
Implant-based breast reconstructive options include tissue expander or permanent implant options, with or without the use of supportive meshes such as an acellular dermal matrix. The advantage of implant options are faster surgery and recovery as well as negating the need for another donor site in the body. The disadvantages include the higher risk of infection, implant extrusion and failure, and capsular contracture. Also, in general, implants are less resistant to radiation therapy.
Own tissue, otherwise known as autologous, options are chosen depending on the type of resection performed as well as the availability of tissue from the patient. In smaller partial breast resections, local tissue rearrangement can be performed to help fill in the resultant dead space with minimal negative aesthetic impact. This is also known as oncoplastic reconstruction.
In larger resections, local tissue rearrangement can lead to obvious differences in size between the normal and reconstructed breasts. These larger partial defects can be reconstructed with fat grafting at a later stage or with local or pedicled flaps. Fat grafts are fat cells, stem cells, and growth factors taken from another part of the body with excess fat using liposuction techniques and injected into the defect area. Due to the fat graft relying on the recipient site for a new blood supply, there is a limit to the amount of fat that can be injected each time. However, fat grafting can be repeated, and can even be used to reconstruct a whole breast over time.
Local and pedicled flaps refer to tissue from the patient’s own body that is shifted into the defect based on that tissue’s own blood supply. This allows for larger amounts of tissue to be used but is dependent on the availability around the defect as well as the length of the blood supply. Smaller local and pedicled flaps include the lateral intercostal artery perforator (LICAP) and thoracodorsal artery perforator (TDAP) flaps, which are commonly used to reconstruct larger partial resection defects. Larger pedicled flaps can be used to reconstruct full mastectomy defects. These larger flaps include the pedicled latissimus dorsi (LD) myocutaneous and the transverse rectus abdominis myocutaneous (TRAM) flaps. Both of these involve the sacrifice of a muscle, although the surrounding muscles can usually compensate for most of the loss of function. Occasionally, fat grafting can be combined with these flaps where larger mastectomy defects need to be reconstructed.
Due to advancements in plastic and reconstructive surgery, free flaps have now become one of the mainstays for breast reconstruction after mastectomy. Free flaps are tissue from other parts of the body, such as the lower abdomen or thigh, which are harvested with their supplying blood vessels intact, then transecting those blood vessels, bringing the tissue to the breast recipient site, and using fine microsurgical techniques to join the flap blood vessels to blood vessels at the recipient site, thus restoring blood flow to the flap. The advantages of free flaps are the wide availability of donor site tissue, with no need for the muscle to be taken, thus reducing morbidity at the donor site. The current gold standard for free flap breast reconstruction is the Deep Inferior Epigastric Perforator (DIEP) flap.
How is DIEP flap surgery performed?
The DIEP flap is skin and fat taken from the abdomen, usually below the belly button, based on blood vessels arising from the deep inferior epigastric artery and vein (DIEA and DIEV) which are part of the blood supply to the abdominal rectus (six-pack) muscles. Using pre-operative investigations and precise techniques, the tiny perforating blood vessels from the DIEA and DIEV supplying the DIEP flap are found and traced through the muscle, thus preserving rectus muscle function and abdominal strength. Once the flap is raised the supplying DIEA and DIEV are transected, and the flap is transferred to the mastectomy site, there the DIEA and DIEV are usually joined with vessels from the internal mammary or thoracodorsal vascular systems. The resultant donor site defect is closed and the umbilicus is brought out through a new position on the skin.
The advantages of the DIEP flap are natural feel and texture, the ability to restore sensation, reduced donor site morbidity, as well as the ability for the flap tissue to counteract the negative effects of radiotherapy. It also helps that the woman gets an attractive, flat abdominal contour after the procedure!
Done in the right hands, success rates of the DIEP flap approach 98-99%, which is consistent with the best centers in the world.
What is the recovery process like after breast reconstructive surgery?
After the surgery, the patient may be placed in a compressive bra which aids in support and swelling reduction. There may be drains from the breast and/or donor site to help remove any excess post-operative blood and fluids. These drains are usually kept for a few days and are removed once the drainage per day is low.
The first day after the procedure is usually spent resting in bed. In the following days, the patient will be sat out of bed and allowed to walk, often with the aid of a physiotherapist. Full, independent ambulation is usually achieved by day 3 or 4 after surgery.
Depending on the type of reconstruction performed, a hospital stay can range from day surgery (for implant reconstructions) to up to a week (for DIEP flap surgery). DIEP flap surgery patients are getting discharged earlier, sometimes even on postoperative day 3. However, this can vary according to the complexity of the surgery and the recovery ability of the patient. The donor site utilized also contributes to the recovery. For example, patients who use tissue from the abdomen, such as in DIEP flap surgery, will feel a tightness in the abdomen for the first few days after surgery and will take about a week or so to reach normal posture. For those who have tissue taken from the back, progressive return to the full range of motion of the affected arm will be introduced.
In general, a full return to activity can be expected at 6-8 weeks after surgery.
Contact Form
1 Orchard Boulevard #10-08 Camden Medical Centre, Singapore 248649
6 Napier Rd, #08-01 Gleneagles Medical Center, Singapore 258499
Tel: +65 6737 4565 | Mobile: +65 8828 4565 | Email: clinic@polarisplasticsurgery.com | Business Hours: Mon - Fri: 9am - 6pm | Sat: 9am - 1pm | Sun/Ph: Closed