Reconstructive Procedures: Breast Reconstruction
Table of Contents
- What is breast reconstruction?
- Who would benefit from breast reconstruction?
- When is breast reconstruction performed?
- How is breast reconstruction performed?
- What happens before surgery?
- During the procedure
- Post-operative care
- Potential risks and complications
- Why choose Polaris Plastic Surgery?
- Conditions and procedures
- Faqs
- References
Breast Reconstruction
What is breast reconstruction?
Who would benefit from breast reconstruction?
When is breast reconstruction performed?
Even if a delayed reconstruction is chosen, your surgeon may recommend the insertion of a tissue expander at the breast resection surgery, as this will help to recruit skin for reconstruction at the time of your definitive reconstructive surgery.
How is breast reconstruction performed?
Traditionally, breast implants have been placed behind the pectoralis major muscle for breast reconstruction. But in recent years and with development in materials such as acellular dermal matrix, placing the implant under the skin and in front of the muscle, (pre-pectoral breast implant reconstruction), which is the natural plane of breast tissue, has gained increasing popularity, and our surgeons are very familiar with these procedures.
Autologous reconstruction borrows tissue from another part of your body to reconstruct the breast and can be performed with the blood supply attached (pedicled reconstruction) or by reattaching the blood supply at the breast (free tissue transfer). Tissue can be taken from many areas where there is excess skin and fat, most commonly the abdomen, but also from the back, thighs, and buttocks. The most common forms of autologous reconstruction are the Deep Inferior Epigastric Perforator (DIEP) and Transverse Rectus Abdominis Myocutaneous (TRAM) flaps, which can either be performed as a pedicled or free flap. Autologous reconstruction provides the most natural and lasting method of reconstruction, but often takes longer and results in donor site scars. These scars, however, can be well hidden.
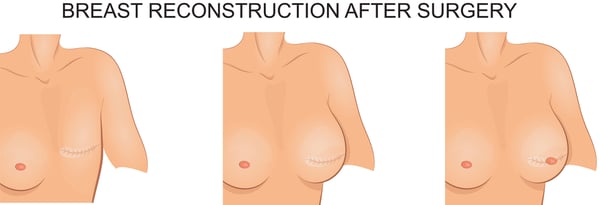
After the initial reconstruction, your surgeon may recommend additional procedures such as nipple reconstruction and other touch-ups to enhance symmetry and appearance. Secondary problems resulting from breast cancer treatment, such as lymphedema and radiation injury, can also be treated at the same time as the reconstructive surgery, or later.
At Polaris Plastic and Reconstructive Surgery, our board-certified plastic surgeon will be happy to perform a thorough assessment and discuss the appropriate options for your breast reconstructive surgery. Dr Adrian is sub-specialist trained in all forms of breast reconstruction and fellowship certified specifically in free DIEP and TRAM flap procedures, areas in which he is well published.
What happens before surgery?
The majority of breast reconstruction surgery is done under general anaesthesia. Various investigations may be done to help with the diagnosis and planning, as well as to optimize you for surgery. If you have any pre-existing medical conditions, you should be optimized for these prior to the operation. Necessary pre-operative blood and radiological tests will be done. If autologous free flap reconstruction is chosen as the modality, you may require a CT-angiogram prior to the operation, which provides a road map for surgery and makes the procedure more efficient.
During the procedure
Post-operative care
Potential risks and complications
More recently, textured implants have been associated with a rare form of lymphoma (BIA-ALCL) which is usually treatable. Thus far, smooth implants have not been implicated. Your surgeon should discuss this phenomenon with you if implant reconstruction is considered. For more information on this, see our FAQ on BIA-ALCL.
Why choose Polaris Plastic Surgery?
Schedule a consultation with our surgeons to assess your needs and goals. They will communicate with you regarding your concerns, and in discussion formulate and perform the appropriate reconstructive procedure for you.
FAQ
Will Medisave/Medishield/private insurance plans cover breast reconstruction?
Yes. Breast reconstruction as well as the follow-up balancing procedures are usually covered by Medisave/Medishield/private insurance plans. The aim of breast reconstruction is to restore the patient’s appearance back to normal.
Does breast reconstruction interfere with breast cancer surveillance?
With adequate clinical and radiological follow up, breast reconstruction does not interfere with breast cancer surveillance.
Can I reconstruct both breasts at the same time?
If bilateral mastectomies are being performed, both breasts can be reconstructed at the same time, either with implants or the patient’s own tissue. The surgical time, as expected, will be longer.
What is Breast Implant Associated Anaplastic Large Cell Lymphoma (BIA-ALCL)?
BIA-ALCL is a rare lymphoma that is associated with breast implants, mostly occurring in patients who have undergone textured-surface breast implants. Since 1997, there have been over 300 cases reported. As this is an uncommon disease, data is still being accumulated and medical knowledge on this topic continues to evolve.
The most common presentation is a late effusion, with breast enlargement more than one year following the breast implant surgery. Other less common symptoms include a breast mass, enlargement of the lymph nodes of the axilla, or fever and night sweats. The average time to onset of BIA-ALCL after implantation is 10 years. BIA-ALCL may affect patients with either silicone- or saline-filled implants.
BIA-ALCL is diagnosed radiologically together fluid aspiration which is sent for testing. If confirmed, further investigations may be required. BIA-ALCL usually presents early, and curative treatment can be performed by implant removal and complete excision of the peri-implant capsule. Unless spread is found, no other treatments are usually needed.
If you already have breast implants, there is no need to change your routine medical care and follow-up. Should you experience any of the symptoms described above, do arrange for a consultation with your plastic surgeon.
2. Ooi A SH, Chang DW. Discussion: Volumetric planning using computed tomographic angiography improves clinical outcomes in DIEP flap breast reconstruction. Plast Reconstr Surg 2016;137:781-782.
3. Park, J. E., Shenaq, D. S., Silva, A. K., Mhlaba, J. M. & Song, D. H. Breast Reconstruction with SIEA Flaps. Plastic and Reconstructive Surgery 137, 1682–1689 (2016).
4. Nealon, K. P. et al. Prepectoral Direct-to-Implant Breast Reconstruction. Plastic and Reconstructive Surgery 145, 898e–908e (2020).
5. hang, D. W. Breast Reconstruction with Microvascular MS-TRAM and DIEP Flaps. Archives of plastic surgery 39, 3–10 (2012).
PATIENT STORIES
Post Massive Weight Loss Body Contouring
A 40-year-old lady consulted with Dr Pek with the desire to correct large amounts of excess skin and soft tissue. She had undergone Bariatric Surgery (Sleeve Gastrectomy) 2 years prior to her presentation and had successfully lost almost 30kg of weight. With ... Read more
Treat Gynecomastia with Minimally Invasive Methods in Singapore
A 38-year-old male engineer presented to Dr Pek with symptomatic growth of his chest/breast area. Since puberty, he complained of unusually prominent chest tissue around his nipple and areolar region. This had worsened gradually over the years, with the left ... Read more
Upper eyelid lift and eyebags rejuvenation
63 years old Chinese female with hypertension and hyperlipidemia presented to Dr Pek with significant droopiness of her upper eyelids on both sides, affecting the upper portion of her visual field. She would constantly feel that her upper eyelids were heavy, ... Read more
Bilateral breast reconstruction using abdominal free flaps
A 45-year-old mother of 2 children was diagnosed with left breast cancer, for which a skin-sparing mastectomy (total removal of breast tissue leaving behind the skin envelope) was recommended. Read more
ARTICLES
TL;DR: A tummy tuck (abdominoplasty) goes beyond aesthetics ...
TL;DR: Lymphedema is long-term swelling caused by poor ...
Contact Form
1 Orchard Boulevard #10-08 Camden Medical Centre, Singapore 248649
6 Napier Rd, #08-01 Gleneagles Medical Center, Singapore 258499
Tel: +65 6737 4565 | Mobile: +65 8828 4565 | Email: clinic@polarisplasticsurgery.com | Business Hours: Mon - Fri: 9am - 6pm | Sat: 9am - 1pm | Sun/Ph: Closed