Articles
How Liposuction & Skin Excision Can Help With Severe Lymphedema Cases
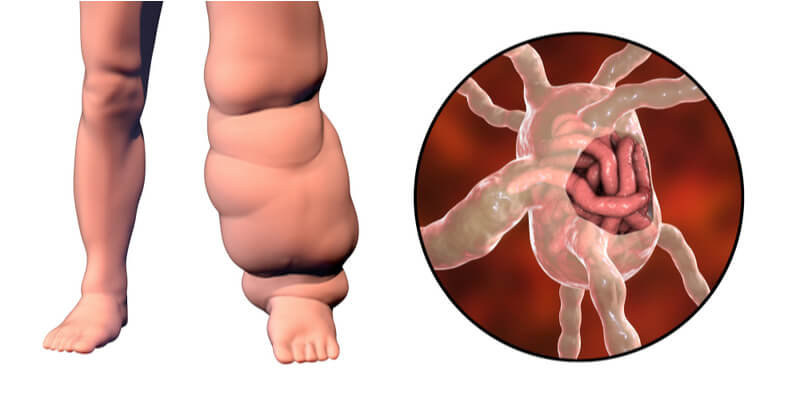
Lymphedema is a chronic, progressive disease affecting mostly the arms and legs that can be extremely functionally debilitating, and eventually lead to disfigurement of the limb if not treated on time. Once skin changes and fat accumulation are established, one of the only ways to reverse the situation is through excisional lymphedema surgery.
Lymphedema in details
Lymphedema is characterized by swelling in the limb which develops as a result of lymphatic fluid accumulation due to an impaired lymphatic transport system. This can be due to any interruption of the lymphatic system, including infection, trauma, and in developed countries such as Singapore, removal of lymph nodes for cancer treatment. In some cases, there is no known cause.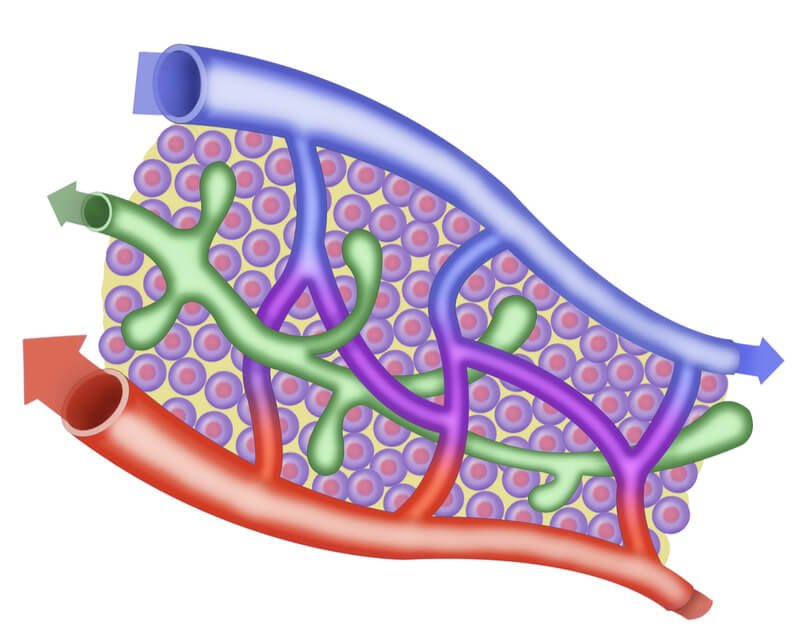
The lymphatic system cleanses our body by draining the excess fluids, toxins, pathogens, and even fat cells from tissues back to the circulation through the lymph vessels. If not drained promptly, this lymphatic fluid rich in toxic and inflammatory substances accumulates and causes pain, swelling, inflammation, recurrent infections, and impaired mobility.
Over time, there is an accumulation of fat in the limb, and the tissue of the limb undergoes fibrosis, leading to permanent damage. This leads to a deformed, disfigured extremity with reduced function.
Treating early or impending lymphedema is also equally important to prevent repeated surgeries or even lymphedema associated disabilities. For this, physiological lymphedema surgery may be the best option.
Managing lymphedema with excisional lymphedema surgery
Conservative management such as manual lymphatic drainage (MLD) or physiological surgical procedures such as lymphaticovenous anastomosis (LVA) and vascularized lymph node transfer (VLNT) can help to manage early and intermediate lymphedema by promoting and restoring fluid drainage from the limb.
If not drained, the chronic lymphedema can stimulate excess and permanent fat growth in the affected limb. Furthermore, fibrosis can take over, along with overlying skin changes and an extremely heavy deformed, debilitating condition called elephantiasis sets in. This form of lymphedema cannot be managed via comprehensive decongestive therapy (CDT), LVA or VLNT.
The role of excisional lymphedema surgery involves removing the excess fat through liposuction, a debulking process. In severe cases that involve fibrosis and trophic skin changes like thickening, acanthosis, recurrent cellulitis and ulceration, a more extensive excisional surgery including both skin and fat excision may be considered.
Lymphedema surgery: With or without skin excision?
Your plastic surgeon may recommend the excisional method in the following cases:
- Confirmed diagnosis of advanced lymphedema with:
- Firm and non-pitting swelling due to excess fats and fibrotic tissues.
- Heavy painful limb restricting mobility or normal functions.
- Chronic, irreversible skin changes in the limb
- Deformed appearance (elephantiasis)
- Non-responsive to conservative CDT and physiological LVA, LNT therapies.
What happens during excisional lymphedema surgery?
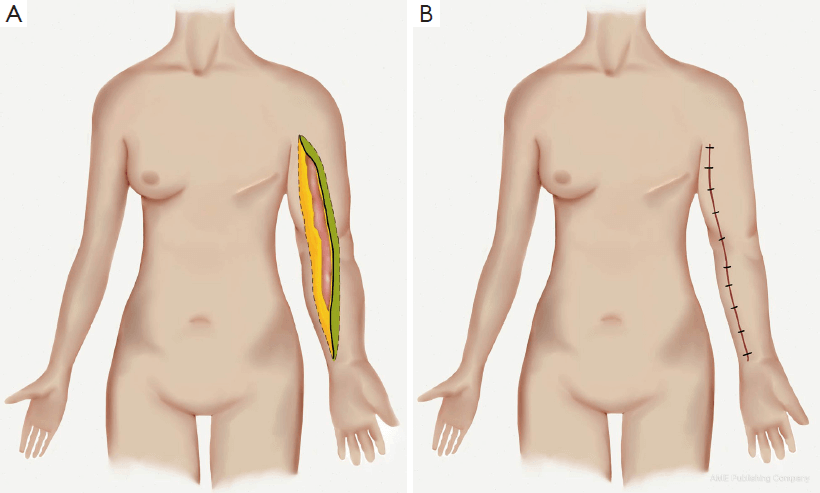
Excisional procedure along the length of extremity (source).
Excisional lymphedema surgery generally includes liposuction and/or surgical excision if needed.
1. Liposuction or “suction-assisted protein lipectomy”
It is an ablative procedure performed only by trained surgeons. Small incisions are made over the swollen area and a specialized cannula is inserted through to dislodge and suck the accumulated fatty tissue. A temporary tourniquet may be used to help limit blood loss.
The surgery is normally performed under general anaesthesia (GA), and begins from the distal end, working upwards and circumferentially in a longitudinal direction to minimize damage to the remaining lymphatics. The incisions are then closed using dissolvable sutures; thus, no suture removal is required.
Following the procedure, compression garments are worn around the treated area for a duration as per your surgeon’s instructions. The advantages of the suction-assisted protein lipectomy procedure for lymphedema imperceptible scars, low morbidity, drastic volume loss, reduction in pain and heaviness, improvement in cosmetic appearance and functioning, as well as increased patient satisfaction, when performed by a qualified plastic surgeon.

2. Skin excision or radical debulking
This procedure is typically performed for advanced or end-stage fibrosclerotic lymphedema and elephantiasis. These conditions are usually associated with skin thickening, ulceration, cellulitis, and severe disfigurement.
The most popular method of skin excision is the Charles’ procedure. Here, the damaged skin and subcutaneous tissue is excised down to the level of deep fascia over the muscles (without injuring the deep fascia). Afterwards, the defect is covered with skin grafting.
Though the results can dramatically improve function, this procedure may be associated with multiple complications like scarring, papillomatosis, wart formation, obliteration of superficial skin lymphatic collaterals, infection and even skin graft failure necessitating regrafting. To avoid them, different modified versions of Charles procedure are practised with successful results, with some of them including combination procedures to maximize the effect and restrict the extent of excision.
How much do you pay for excisional lymphedema surgery?

The cost incurred for excisional lymphedema surgery is dependent on the affected site, size, amount of fat accumulated, associated skin lesions, infections and even the experience of the surgeon.
Additionally, lymphedema surgeries are usually insurance claimable. Different insurance providers offer different coverage for your lymphedema surgery; thus, it is important to check with your provider about the type of coverage that you will receive.
Severe lymphedema can be painful and incapacitating. Though not fully curable, mild, severe, and advanced forms of lymphedema can be well managed for a better quality of life. Speak to our board-certified plastic surgeon Dr Adrian Ooi who is fellowship specialized in lymphedema to learn more about your options today.
Frequently Asked Questions (FAQs)
Q. Can excision lymphedema surgery completely cure advanced lymphedema?
No, it is a palliative surgery which reduces the swelling volume and improve the symptoms like heaviness, pain, deformity, immobility, etc. but the basic defect of lymphatic system dysfunction remains as it is.
Q. Who should not do lymphedema liposuction?
Someone with:
- Lymphedema responsive to elevation, massage, CDT, LVA, LNT.
- Metastatic cancers.
- Pitting edema as it indicates fluid and not fat.
- Non-compliant patients as post-op care with 24-hours compression is essential, ignoring which can lead to negative side-effects.
- Open wounds.
- Blood coagulation disorders.
- Not healthy enough to undergo surgery.
Q. What is required for after-surgery care?
- Proper wound care: Regular cleaning and dressing till the wounds heal completely to prevent infections.
- Wear 24- hour compression garments: only to be removed once a day for bathing and changing the garment.
- Proper moisturization of skin: to prevent excessive drying and decrease the risk of infection.
- Regular change of compression garments as per the change in size of swelling.
- Maintain good hygiene.
- Regular follow-up.
Q. Are there any side-effects associated with excisional lymphedema surgery?
- One may develop bruising, mild swelling, numbness, or pain immediately after the liposuction procedure which resolves with time.
- Skin irritation due to compression garments.
- Incision scars may persist.
- Unevenness of skin due to fat removal can be seen.
- Multiple procedures may be needed for large areas of treatment.
- Serious complications like infections, DVT, Pulmonary embolism or fat emboli are rare but not impossible.
Q. How is lymphedema different from lipedema?
Lymphedema is the accumulation of lymphatic fluid superseded by fats whereas lipedema is the deposition of pathological fat.
| Lymphedema | Lipedema |
| Mostly unilateral | Mostly symmetrical |
| Defective lymphatic drainage | Hormonal changes |
| Swelling and heaviness reduces with fall in weight | Swelling not affected by weight changes |
| Swelling reduces with limb elevation. | No effect of limb movement. |
| No hypersensitivity or tenderness seen. | Affected area tenderness and hypersensitivity present. |
| Overlying skin can be thick, firm, inflamed or scarred. | Overlying skin is normal and soft |
Contact Form
1 Orchard Boulevard #10-08 Camden Medical Centre, Singapore 248649
6 Napier Rd, #08-01 Gleneagles Medical Center, Singapore 258499
Tel: +65 6737 4565 | Mobile: +65 8828 4565 | Email: clinic@polarisplasticsurgery.com | Business Hours: Mon - Fri: 9am - 6pm | Sat: 9am - 1pm | Sun/Ph: Closed