Reconstructive Procedures: Lymphedema Surgery

Table of Contents
- What is lymphedema
- What are the clinical features of lymphedema?
- What treatments are there for lymphedema?
- How can surgery help with lymphedema?
- What happens before surgery?
- During the procedure
- Post-operative care
- Potential risks and complications
- Why choose Polaris Plastic Surgery?
- Procedures
- Faqs
- References

What is lymphedema?
What is lymphedema?
Lymphedema is the abnormal accumulation of fluid in the compartments of the body due to dysfunction in the lymphatic system. This can be primary, where there is an inherent underlying problem with the lymph vessels or nodes, or secondary, where an infection, trauma, surgery or even radiation has resulted in a disruption to the lymphatic flow. The most common cause of lymphedema in developed nations is cancer treatment-related. This is either due to surgery to the lymph node basins, or from radiotherapy causing damage to the lymphatic system. For example, up to 30% of patients who have received breast cancer treatment and axillary lymph node clearance will develop lymphedema in their lifetime.
What are the clinical features of lymphedema?
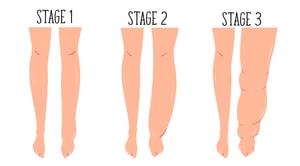
The International Society of Lymphangology (ISL) classified lymphedema into 3 stages according to the clinical features. Briefly, they are:
What treatments are there for lymphedema?
In terms of medication, therapies such as diuretics to offload fluid from the body have been tried, without much success. Moreover, if used in excess these diuretics can lead to imbalances in the body’s electrolytes and even kidney problems.
In the past decade, surgical treatments for lymphedema have garnered increasing attention and have improved significantly. Most of the developments have been in physiological treatments aimed at restoring the dysfunctional lymphatic system and include lymphaticovenous bypass/anastomosis (LVB/LVA) surgery and vascularized lymph node transfer (VLNT).
How can surgery help with lymphedema?
For VLNT, lymph nodes are taken from a part of your body where lymph nodes are in excess and transplanted to the affected limb. In select patients, VLNT can be performed together with other procedures such as extremity or breast reconstruction to achieve dual aims simultaneously. VLNT procedures usually require a few days of hospital stay and about 1 to 2 weeks downtime.
In severe cases of ISL stage 3 lymphedema, physiological techniques may no longer be possible due to the amount of fibrosis and skin changes. For these situations, excisional surgery such as liposuction or removal of fibrotic skin can be performed to debulk the affected body part.
Post-surgery, patients will still have to continue taking care of their lymphedema, as none of these treatments can be said to be 100% effective. However, many patients report reduced symptoms and weight of the affected limb, and there are some who completely stop lymphedema therapy altogether.
What happens before surgery?

To aid in the diagnosis of lymphedema and to stage the severity of the condition, your doctor may order advanced imaging techniques such as lymphoscintigraphy, indocyanine green lymphangiography, and MR-lymphangiography. These investigations will help confirm the diagnosis of lymphedema, as well as plan for potential surgical interventions. In addition, certain pre-operative blood tests and X-rays may be performed if surgery is planned.
During the procedure
Post-operative care

Potential risks and complications
Why choose Polaris Plastic Surgery?
Schedule a consultation with one of our surgeons to assess your needs and goals. He will communicate with you regarding your concerns, and in discussion formulate and perform the reconstructive procedure for appropriate outcomes.
Procedures
FAQ
What is lipedema? How is it different from lymphedema?
Lipedema is the abnormal accumulation of subcutaneous fat in the body. It can cause social embarrassment, difficulty walking, and can even be painful. Whilst obesity can also cause fatty accumulation, lipedema predominantly affects only the buttocks and the legs, with the rest of the body being of normal size. It is refractory to exercise and diet, and affects only women, with incidences reported at up to 11%. Physiological lymphedema techniques are ineffective for pure lipedema, which usually requires liposuction or excisional techniques to treat. However, in some cases, both conditions can co-exist. See a specialist plastic surgeon who is trained in these techniques and he can advise you accordingly.
Will I need to continue wearing my pressure garments for lymphedema post-operatively?
The short answer is yes. Lymphedema surgery does not treat 100% of the condition, therefore it is always recommended to continue your lymphedema maintenance and garments post-operatively. However, there are some patients who, after a while, find that they no longer need their pressure garments.
2. Chang, D. W., Suami, H. & Skoracki, R. A Prospective Analysis of 100 Consecutive Lymphovenous Bypass Cases for Treatment of Extremity Lymphedema. Plastic and Reconstructive Surgery 132, 1305–1314 (2013).
3. Garza, R., Ooi, A., Falk, J., Chang, D. (2019). The Relationship Between Clinical and Indocyanine Green Staging in Lymphedema Lymphatic Research and Biology 17(3), 329-333.
4. Nguyen, A., Chang, E., Chang, D. (2013). Simultaneous Vascularized Lymph Node Transfer with Microvascular Breast Reconstruction Plastic and Reconstructive Surgery 132(), 22.
PATIENT STORIES
Post Massive Weight Loss Body Contouring
A 40-year-old lady consulted with Dr Pek with the desire to correct large amounts of excess skin and soft tissue. She had undergone Bariatric Surgery (Sleeve Gastrectomy) 2 years prior to her presentation and had successfully lost almost 30kg of weight. With ... Read more
Treating Gynecomastia – Correct Male Breasts through minimally invasive techniques
A 38-year-old male engineer presented to Dr Pek with symptomatic growth of his chest/breast area. Since puberty, he complained of unusually prominent chest tissue around his nipple and areolar region. This had worsened gradually over the years, with the left ... Read more
Upper eyelid lift and eyebags rejuvenation
63 years old Chinese female with hypertension and hyperlipidemia presented to Dr Pek with significant droopiness of her upper eyelids on both sides, affecting the upper portion of her visual field. She would constantly feel that her upper eyelids were heavy, ... Read more
Bilateral breast reconstruction using abdominal free flaps
A 45-year-old mother of 2 children was diagnosed with left breast cancer, for which a skin-sparing mastectomy (total removal of breast tissue leaving behind the skin envelope) was recommended. Read more
ARTICLES
Let's be real, we all have those areas of our body where ...
Rhinoplasty, commonly known as a nose job, is a surgical ...
Plastic reconstructive surgery is a specialised field that ...
Droopy eyelids are not just a cosmetic concern. While it ...
Contact Form
1 Orchard Boulevard #10-08 Camden Medical Centre, Singapore 248649
6 Napier Rd, #08-01 Gleneagles Medical Center, Singapore 258499
Tel: +65 6737 4565 | Mobile: +65 8828 4565 | Email: clinic@polarisplasticsurgery.com | Business Hours: Mon - Fri: 9am - 6pm | Sat: 9am - 1pm | Sun/Ph: Closed