Articles
LVB/LVA Bypass Surgery for Lymphedema Treatment in Singapore
The lymphatic system, alongside the veins, helps fluid flow back towards the heart as part of the body’s circulatory system. Specifically, it helps the flow of fat cells and enables the removal of toxins and infectious organisms. Any blockage or disruption in this lymphatic transport system leads to stagnation of lymph fluid causing swelling known as lymphedema, and this can be treated with a lymphaticovenous bypass surgery (LVB).
This usually involves the upper and lower limbs, which can balloon up causing pain, infection and loss of mobility and function. One of the best ways to drain this fluid is to bypass the blockage by diverting the lymphatic flow into the neighbouring venous system. This surgical technique for treating lymphedema is known as lymphaticovenous bypass surgery.
What is Lymphaticovenous Bypass/Anastomosis Surgery (LVB/LVA)?
Lymphaticovenous bypass/anastomosis (LVB/LVA) involves supramicrosurgery in which the blocked lymphatic vessel of an affected limb is connected to a nearby vein with the aid of ultra-fine instruments and a powerful operating microscope. This bypass allows the accumulated excess lymph fluid to flow through the vein and ultimately re-enter the body’s natural circulation.
It is an advanced physiological surgical technique which provides an alternative route for lymph to flow and thus reduce or prevent the recurrence of lymphedema. It is especially helpful in the early phases of the disease. A good analogy would be that of a traffic jam on an expressway (the lymphatic system). By building a connection to a neighbouring expressway which is not jammed, the traffic flow can be restored. This connection is the LVB.
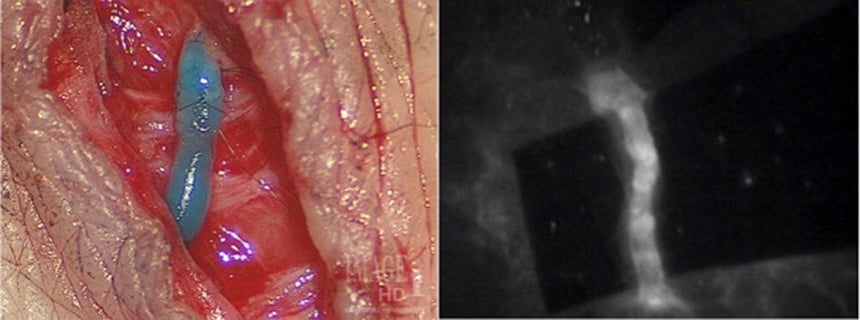
Figure showing the lymphaticovenous bypass procedure (source).
What kind of lymphedema condition can LVB/LVA treat?
In early phase lymphedema, conservative treatments like leg elevation, daily massaging, high-quality gradated elastic compression stockings, and physiotherapy may help. When these fail to show satisfactory results, the next stage would be physiological lymphedema surgery.
LVB/LVA restores the physiological flow of accumulated lymphatic fluid, with results best seen in cases where lymphedema has not led to any chronic skin changes or fatty accumulation (latent and early stages). In the later stages of lymphedema (moderate and severe lymphostatic elephantiasis), swelling is mostly composed of fat and fibrous tissues, and the patient may not benefit from using LVB/LVA techniques, and thus, require excisional rather than physiologic surgery.
For LVB/LVA to be effective, the lymphatic vessels should be healthy and functional to pump out enough lymphatic fluid. Skin damage and tissue changes should be minimal (such as thickening or hardness).
How is lymphaticovenous anastomosis surgery performed?
Pre-operative phase
- Lymphatic channel selection by lymphatic mapping (ICG lymphography)
The LVB/LVA surgery is most effective for patients with functional and healthy lymphatic ducts. To check the functionality of lymphatics, a small amount of indocyanine green dye (ICG) is injected intradermally on the dorsum (upper part) of the corresponding foot or hand prior to the surgery.
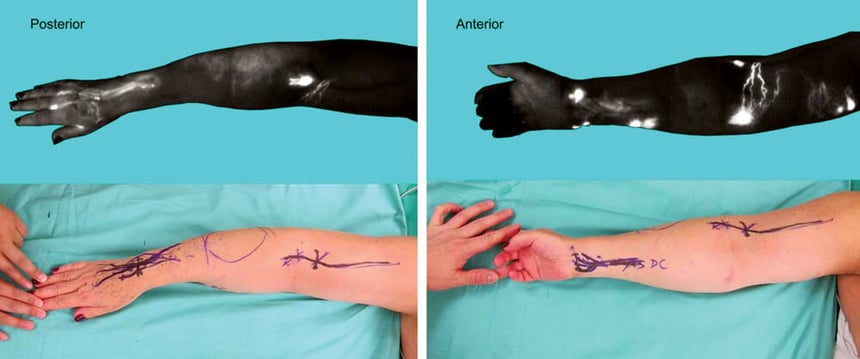
Using ICG lymphography to identify functioning ducts (source).
This dye travels through the lymphatic system and moves along the lymphatic drainage to form different patterns. These patterns can be easily visualised in real-time with infrared cameras, showing how well the lymphatic vessels are working. This way, the appropriate lymphatic ducts for LVBs can be identified.
During the surgery
Surgery can be performed either under general anaesthesia or local anaesthesia with sedation.
This surgery is performed under microscopic magnification for enhanced precision. The reconstructive technique begins with a small skin incision to identify the lymphatic vessel and an adjacent vein.
With the help of ultra-fine super-microsurgical instruments, the lymphatic vessel and vein are connected, bypassing the blockage and allowing the excess fluid to drain properly into the vein. As many connections as possible are made at multiple points up and down the limb. Each of these connections acts as a low pressure exit point for the lymph to flow into the circulatory system.

Postoperatively, the extremity is wrapped in a compressive bandage in an extended position.
Post-surgery
LVBs are a relatively low-risk procedure and the patient can be discharged on the same day itself. The limb will be wrapped for the first few weeks, before returning to compression garments. The lymphedema therapist plays a key role in this stage of the recovery.
Along with decreased pressure and limb girth, patients may also notice a reduction in swelling, pain, infective episodes and the use of compression garments over time, with increased comfort, function and overall well-being.
Your lymphedema specialist will also provide you with further aftercare instructions, as well as have your follow-up appointments scheduled to monitor your progress.
How much does an LVB/LVA surgery cost in Singapore?
The cost for LVB/LVA lymphedema surgery in Singapore may differ from patient to patient. Surgeons will take into account the gravity of the condition, surgical facilities, surgeon’s fees and more.
Are there other alternatives to lymphaticovenous bypass surgery?
There are various management options to treat different phases of lymphedema, such as vascularized lymph node transfer (VLNT) or excisional lymphedema surgery.
VLNT is also physiological surgical technique. It also utilizes microsurgery, and can be used in isolation or concurrent with LVBs treat latent, mild and moderate lymphedema.
However, in contrast to LVB/LVA, the VLNT technique involves connecting an entire cluster of functional lymph nodes along with its blood supply. The lymph nodes are taken from an area of excess and brought to the affected region (recipient site), with both the artery and vein supplying the lymph nodes anastomosed with the corresponding vessels at the recipient site. Through direct connection or the release of growth factors, lymphatic ducts then grow into the lymph nodes, with the vein of the VLNT removing excess lymph fluid.

Our board-certified consultant plastic surgeon and lymphedema specialist Dr Adrian Ooi can help to guide you through your options to treat lymphedema. Schedule an appointment with us to understand more about these treatments.
Frequently Asked Questions (FAQs)
Q. What are the different types of lymphedema?
There are 2 types of lymphedema.
- Type 1 (Primary lymphedema): It is present since birth and can be genetic. Here, part of the lymphatic system might be absent, not fully developed, defective or hypofunctional.
- Type 2 (Secondary lymphedema): This can be due to surgical removal of lymph nodes, recurrent infections, filariasis, chronic venous insufficiency, obesity, etc.
Q. What are the different stages of lymphedema?
- Latency or Subclinical Stage (0): May be asymptomatic, but some signs may include mild heaviness and tightness in the limb, or a reduced transport capacity of the lymphatic system.
- Mild (1): Signs may include early accumulation of protein-rich lymphatic fluid, pitting oedema, and swelling or oedema that is reversible with limb elevation or compression.
- Moderate (2): Signs may include an accumulation of protein-rich lymphatic fluid, no pitting, dermal fibrosis, and swelling that does not subside with elevation or compression.
- Severe (3): Signs may include lymphostatic elephantiasis, heavy limbs, no pitting, trophic skin changes such as acanthosis, fat deposits, papillomatosis, and hyperkeratosis, visible disfiguration, and swelling that consists of fat and fibrosed tissues.
Q. Are there any complications associated with LVA?
Though rare, but possible complications may include infection, poor wound healing, allergy reactions to ICG, or complications due to anaesthesia.
Q. Who cannot undergo LVA surgery?
Someone with:
- Non-functioning lymphatic ducts.
- Severe non-pitting oedema wherein fluid is replaced by fats and fibrosis.
- Deep vein thrombosis or severe varicose veins involving the affected limb.
- Recent infections like cellulitis of the skin of the affected limb.
- Recent treatment for cancers like chemotherapy or radiotherapy.
- Recent treatment for skin cancer of the affected limb.
- Allergic to ICG dye (relative contraindication).
Q. What are the others ways to treat lymphedema?
Non-surgical conservative measures like complete decongestive therapy in the form of leg elevation, compression bandage, manual drainage therapy, weight loss and physiotherapy can relieve swelling and support the pumping actions of lymphatic vessels in mild cases.
Excisional lymphedema surgery comprising of liposuction and skin excision is needed in extreme cases when there is mainly excess fat and chronic skin changes.
Contact Form
1 Orchard Boulevard #10-08 Camden Medical Centre, Singapore 248649
6 Napier Rd, #08-01 Gleneagles Medical Center, Singapore 258499
Tel: +65 6737 4565 | Mobile: +65 8828 4565 | Email: clinic@polarisplasticsurgery.com | Business Hours: Mon - Fri: 9am - 6pm | Sat: 9am - 1pm | Sun/Ph: Closed